The International Journal of Oral & Maxillofacial Implants, Pre-Print
DOI: 10.11607/jomi.105365. Apr. 2024,Seiten: 1-36, Sprache: EnglischKrennmair, Gerald / Yalcin, Schwarze Uwe / Weinländer, Michael / Forstner, Thomas / Michael, Michael / Krennmair, Stefan
Objective: The aim of the present study was to compare the histomorphometrically evaluated
new bone formation (NB), the radiographically measured graft stability and the clinical
implant outcome for maxillary sinus augmentation grafted with deproteinized bovine bone
mineral (DBBM) with either small (Bio-Oss-S.) or large (Bio-Oss-L.) particles.
Materials and Methods: By using a split-mouth study design bilateral maxillary sinus
augmentation was performed in 13 patients either with Bio-Oss-S. particles (0.25-1 mm) or
with Bio-Oss-L. (1-2 mm). After a healing period of 6 months bone biopsies were axially
retrieved in the molar region for histologic/histomorphometric analysis of new bone formation
including subsequent staged-implant placement. For determining graft stability the maxillary
sinus augmentation vertical graft heights were radiographically measured immediately after
sinus augmentation, at implant placement and at the 2- and 4-year post-augmentation follow
ups. In addition, the clinical implant-prosthodontic outcome (survival/success/marginal bone
loss) was assessed at year 1 and year 3post-loading.
Results: 22 sinuses of 11 patients with split-mouth evaluation were ultimately available for
data and statistical analysis. Histomorphometric analysis of the axially retrieved bone biopsies
revealed new bone formation (S.:25.5Å}7.0% vs. L.:23.6Å}11.9%; p=0.640), residual graft
(S.:19.6Å}9.2% vs. L.:17.5Å}6.3%; p=0.365) as well as connective tissue (S.:54.9Å}9.2% vs.
L.: 58.9Å}12.5%; p=0.283) without differences between the use of small (Bio-Oss-S.) and
large (Bio-Oss-L.) particles. However, there was significantly (p=0.021) higher graft-to-bone
contact (BGC) for the small-particle ( 27.9Å}14.8%) than for the large-particle size
(19.9Å}12.9%) representing a significantly higher osteoconductivity. Both particles showed
significant (p<0.01) vertical graft height reduction over time (4 years) of about 10% with
predominant graft reduction in the time-period between sinus augmentation and implant
placement compared to the time-period of the follow-ups post implant placement. At the 3-
year post-loading implant evaluation all implants and prostheses survived (100%) and the
peri-implant marginal bone loss (S.:0.52Å}0.19 mm; L.:0.48Å}0.15 mm) as well as the periimplant
health conditions (S.:87.5%, L.:81.2%) also did not differ between implants
inserted with the two different xenograft particles used.
Conclusions: The use of small and large bovine xenograft particles for maxillary sinus
augmentation provides for comparable bone formation ensuring stable graft dimensions
combined with high implant success and healthy peri-implant conditions. However, small
particle size resulted in a higher bone-to-graft contact providing for higher osteoconductivity
than with the larger particle size.
Implantologie, 1/2024
Seiten: 49-62, Sprache: DeutschKrennmair, Gerald / Weinländer, Michael / Forstner, Thomas / Krennmair, Stefan / Stimmelmayr, Michael / Malek, Michael
Eine prospektive klinische StudieIn dieser Studie sollte die Eignung der bukkalen teilschichtigen Eversionsperiostplastik (EPP) für den Weichgewebeverschluss nach horizontalen Kammaugmentationen im Unterkiefer-Seitenzahnbereich untersucht werden, die als Onlay-Transplantation in Knochenschild-Technik durchgeführt wurden. Insgesamt 16 Patienten (12 Frauen und 4 Männer, mittleres Alter: 46,2 ± 8,7 Jahre) mit 18 horizontalen Knochendefekten im Unterkiefer-Seitenzahnbereich wurden inkludiert und erhielten eine laterale Onlay-Knochentransplantation in Knochenschild-Technik. Nach der lateralen Kammaugmentation wurde der Weichgewebeverschluss durch eine EPP hergestellt, die anschließend prospektiv nachbeobachtet wurde. Der Verlauf der Wundheilung wurde mit einem modifizierten Index bewertet. Dieser bestand in einer binären Bewertung (ja = 0, nein = 1) folgender Punkte: (1) Blutung auf Palpation oder spontan, (2) Farbunterschied des Weichgewebes, (3) Präsenz eines Hämatoms, (4) Präsenz von Granulationsgewebe, (5) unvollständiger Schluss der Inzisionsränder, (6) Dehiszenz mit sichtbarem Augmentationsmaterial, (7) Exsudation, (8) Eiterung. Zusätzlich erfolgte eine individuelle Quantifizierung des Schmerzes und der Schwellung mit einer 6-stufigen visuellen Analogskala (VAS, 0 = kein Schmerz/keine Schwellung, 5 = starker Schmerz/starke Schwellung). VAS-Werte von 0, 1 und 2 wurden als 1, VAS-Werte von 3, 4 und 5 als 0 in den binären Heilungsindex eingerechnet. Ein alle 10 Punkte umfassender Summenscore der Heilung wurde 2, 7 und 14 Tage sowie 1 und 4 Monate postoperativ ermittelt und die Ergebnisse der einzelnen Nachuntersuchungen wurden verglichen. Der Summenscore nahm von Tag 2 (6,6 ± 1,1) bis Tag 7 (8,9 ± 1,0) signifikant zu (p < 0,01), zeigte aber zwischen Tag 14 (9,6 ± 0,6) und der 1- und 4-Monats-Nachuntersuchung (10,0 ± 0) nur noch geringe Veränderungen. Weder trat eine Wunddehiszenz noch ein unvollständiger Schluss der Wundränder auf. Im Einzelnen waren Palpationsbluten, Hämatom und Exsudation mit 50 %, 100 % bzw. 22,2 % an Tag 2 und mit 16,7 %, 55,6 % bzw. 22,2 % an Tag 7 die häufigsten Begleiterscheinungen. Die durchschnittlichen VAS-Werte für Schmerz und Schwellung lagen am Tag 2 zunächst bei 4,0 ± 0 bzw. 3,0 ± 0,77, nahmen bis zum Tag 7 (2,0 ± 0 bzw. 2,0 ± 0,59) und Tag 14 (1,0 ± 0,42 bzw. 2,0 ± 0,79) signifikant ab (p < 0,001) und lagen nach 1 und 4 Monaten jeweils bei 0. Die bukkale teilschichtige EPP erleichtert die Lappenverschiebung und ermöglicht einen dichten Weichgewebeverschluss über großen horizontalen Kammaugmentationen im Unterkiefer-Seitenzahnbereich, da ein doppelschichtiger überlappender Wundverschluss erfolgt. Obwohl die Technik chirurgisch anspruchsvoll ist, kann sie die Rate postoperativer Komplikationen signifikant reduzieren.
Originalpublikation: Krennmair G, Weinländer M, Thomas F, Krennmair S, Stimmelmayr M, Malek M. Efficacy of Labial Split-Thickness Eversion Periosteoplasty for Soft Tissue Management in Posterior Mandibular Horizontal Ridge Augmentation Procedures: A Prospective Clinical Study. Int J Oral Maxillofac Implants 2023;38:717–726.
Schlagwörter: Weichgewebeschluss, laterale Knochenaugmentation, Unterkiefer-Seitenzahnbereich
The International Journal of Oral & Maxillofacial Implants, 4/2023
DOI: 10.11607/jomi.10135, PubMed-ID: 37669517Seiten: 717-726, Sprache: EnglischKrennmair, Gerald / Weinländer, Michael / Thomas, Forstner / Krennmair, Stefan / Stimmelmayr, Michael / Malek, Michael
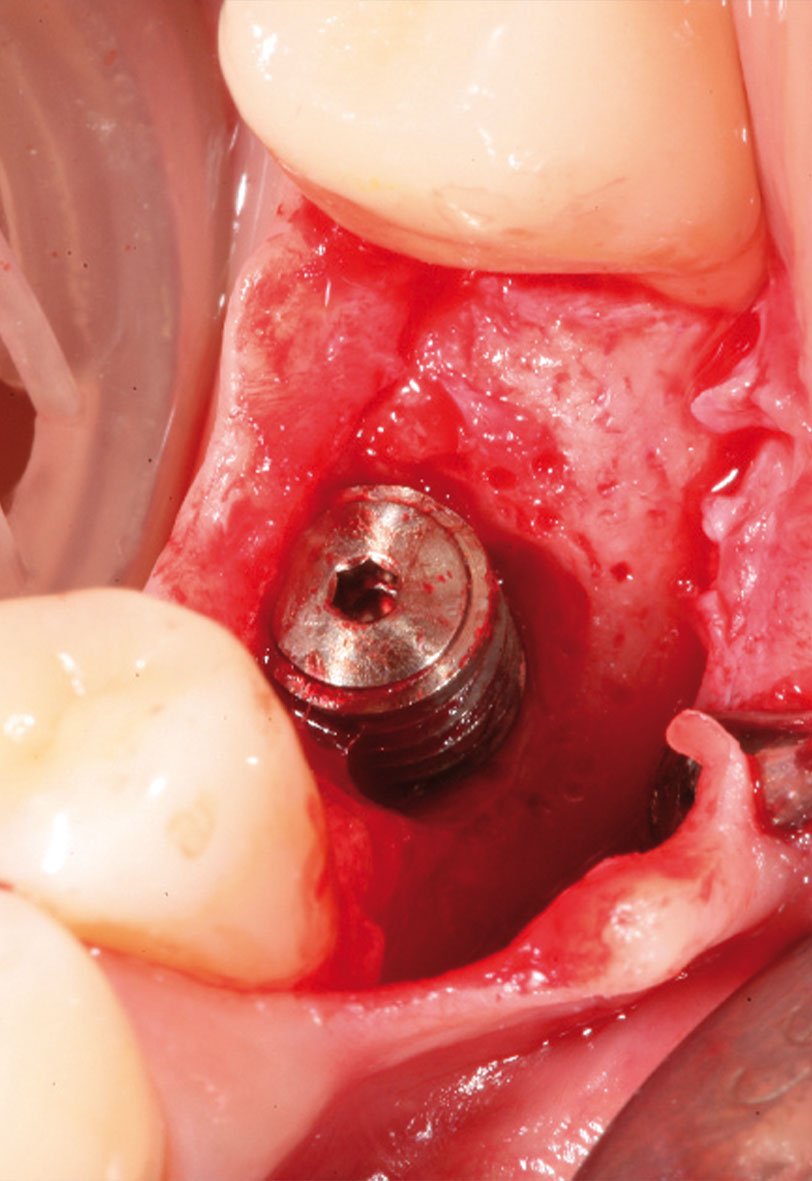
Purpose: To evaluate the efficacy of split-thickness labial eversion periosteoplasty (EPP) for soft tissue closure in horizontal ridge augmentation of posterior mandibular regions using a bone shell onlay grafting technique.
Materials and Methods: Sixteen patients (12 female and 4 male; mean age: 46.2 ± 8.7 years) with 18 horizontal bone defects in posterior mandibular regions were included for lateral onlay bone grafting using the bone shell technique. After lateral bone augmentation, the EPP was used for soft tissue closure and was prospectively followed up for wound healing efficacy using a modified scoring index. The scoring index included dichotomous (yes: 0 / no: 1) evaluation of the following items: (1) bleeding on palpation or spontaneously, (2) tissue color difference, (3) presence of hematoma, (4) presence of granulation tissue, (5) incomplete incision margin closure, (6) dehiscence with visible augmentation material, (7) presence of exudation, and (8) presence of suppuration. In addition, a visual analog scale (VAS) was used to quantify and record the amount of pain and swelling (0 = no pain/swelling and 5 = severe pain/swelling); VAS scores of 0, 1, and 2 were rated as 1 in the dichotomous scoring index, and VAS scores of 3, 4, and 5 were rated as 0. A summarized wound healing score consisting of all 10 items was assessed at days 2, 7, and 14 and at months 1 and 4 postoperatively, including a comparison of the follow-up evaluations.
Results: The summarized healing score increased significantly (P < .01) between day 2 (score: 6.6 ± 1.1) and day 7 (score: 8.9 ± 1.0) but showed little difference between day 14 (score: 9.6 ± 0.6) and the 1- and 4-month follow-ups (score: 10.0 ± 0). There was no wound dehiscence and no incomplete incision margin adaptation. For the individual parameters evaluated, bleeding on palpation, hematoma, and exudation were the most frequent side effects at day 2 at 50%, 100%, and 22.2%, respectively, and at day 7 at 16.7%, 55.6%, and 22.2%, respectively. The average pain score and the swelling/edema score were initially 4.0 ± 0 and 3.0 ± 0.77 on day 2, with a significant decrease (P < .001) by day 7 (pain: 2.0 ± 0; edema/swelling: 2.0 ± 0.59) and day 14 (pain: 1.0 ± 0.42; edema/swelling: 2.0 ± 0.79) and complete absence (score: 0) at months 1 and 4.
Conclusions: Labial split-thickness EPP facilitates flap advancement and enables tight soft tissue coverage in large horizontal posterior mandibular bone augmentations as a result of offset double-layer wound closure. Although this procedure is shown to be surgically demanding, the postoperative complication rate may be reduced significantly.
Schlagwörter: soft tissue closure, lateral bone augmentation, posterior mandible
The International Journal of Oral & Maxillofacial Implants, 4/2020
DOI: 10.11607/jomi.7916, PubMed-ID: 32724933Seiten: 789-798, Sprache: EnglischKrennmair, Stefan / Malek, Michael / Forstner, Thomas / Krennmair, Gerald / Weinländer, Michael / Hunger, Stefan
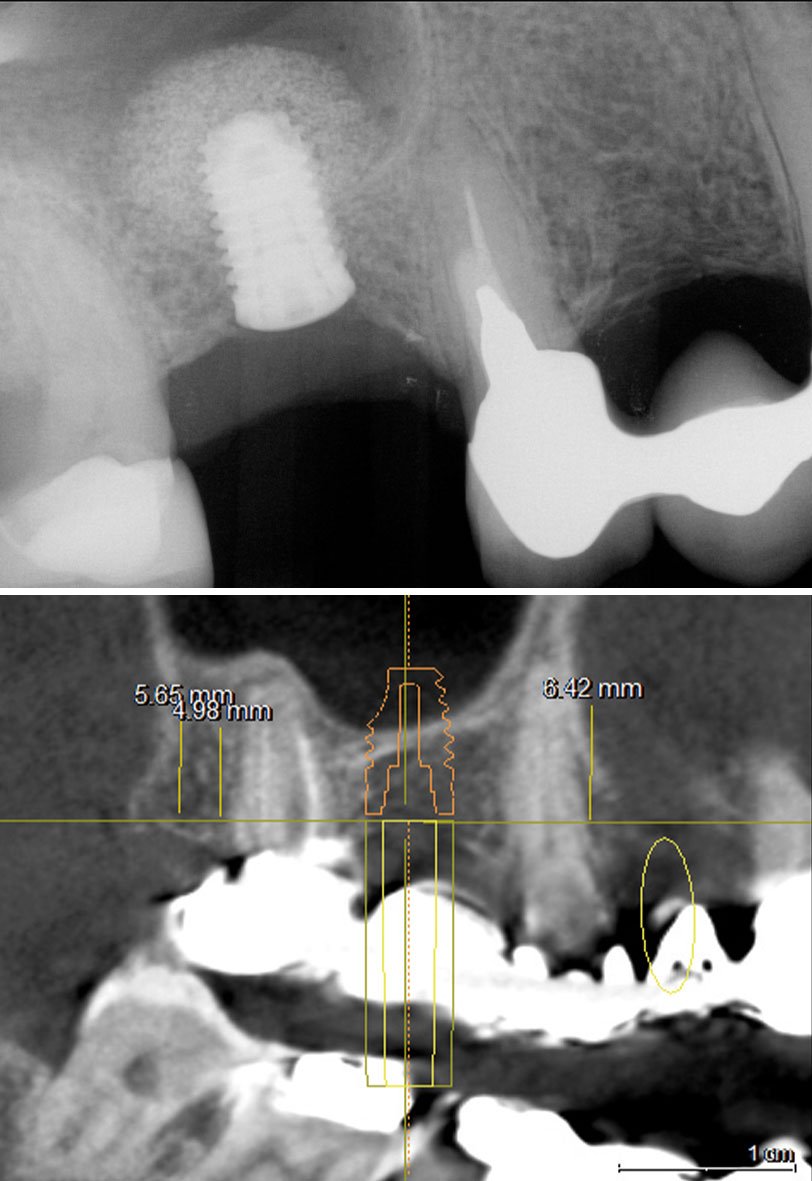
Purpose: To analyze risk factors affecting sinus membrane perforation (SMP) during sinus floor elevation (SFE) procedures using the lateral window technique (LWT).
Materials and Methods: For patients with SFEs using the LWT, patient-related risk factors (age/sex/smoking/diabetes) and surgical-anatomical–related risk factors (stage approach/sinus side/residual ridge height/sinus membrane thickness/previous surgical interventions) were compared between perforated and nonperforated sites and were evaluated for their influence affecting SMP. Additionally, SMPs were further subdivided into small/moderate (< 10 mm) or large (≥ 10 mm) in dimension, which were also analyzed for risk factors and consecutively for their influence on perforation.
Results: The study sample comprised 434 SFE procedures in 355 patients; 94/355 patients (26.5%) presented SMP in 103 of 434 SFE procedures (23.8%). SFE procedures with (n = 103) and without (n = 331) SMP did not differ for patient-related risk factors but differed significantly (P = .001) for surgical-anatomical factors as follows: residual ridge height (3.05 ± 1.35 mm vs 4.15 ± 1.46 mm), sinus membrane thickness (1.2 ± 0.5 mm vs 2.6 ± 1.1 mm), prevalence of staged procedures (78.6% vs 57.7%), presence of maxillary sinus septa (75.7% vs 14.2%), presence of thin (< 1.5 mm) mucosa biotype (62.1% vs 29%), and previous oral surgical interventions (37.9% vs 16.3%). In the multivariate analysis, significant associations of SMP were found with the presence of sinus septa (odds ratio [OR] = 31.992; P = .001), residual ridge height (OR = 1.563; P = .007), sinus membrane thickness (OR = 1.057; P = .001), presence of thin (< 1.5 mm) sinus biotype (OR = 8.883; P = .001), previous surgical interventions (OR = 4.689; P = .002), and smoking habits (OR = 2.238; P = .030). For inducing a large (≥ 10 mm) SMP, the presence of thin sinus membrane thickness/thin sinus membrane biotype (OR = 5.319; P = .006; OR = 22.222; P = .001) and reduced alveolar ridge height (OR = 0.629; P = .026) were assessed as being significant risk factors.
Conclusion: In general, the presence of sinus septa, thin sinus mucosa, staged procedures, and previous surgical interventions are the main risk factors inducing SMP for SFE using the LWT. In particular, the presence of thin sinus membrane in conjunction with a staged procedure significantly increases the risk for a large SMP.
Schlagwörter: lateral window, membrane perforation, perforation size, risk factors, sinus elevation
The International Journal of Oral & Maxillofacial Implants, 6/2018
DOI: 10.11607/jomi.6765, PubMed-ID: 30427967Seiten: 1351-1361, Sprache: EnglischKrennmair, Stefan / Weinländer, Michael / Malek, Michael / Forstner, Thomas / Krennmair, Gerald / Stimmelmayr, Michael
Purpose: To evaluate the 5-year clinical outcomes for implants placed in a staged sinus floor elevation (SFE) procedure and to compare three patient groups with sinus grafts with three different ratios of bovine bone mineral (BBM) and autogenous bone (AB) mixture.
Materials and Methods: A 5-year prospective cohort study was conducted on 81 patients with 119 staged SFEs non-randomly distributed to three groups based on the origin of the AB and the mixture ratio with BBM: group 1 (locally harvested AB [LHB] from osteotomy sites + BBM, ratio: 1:10), 31 patients, 37 SFEs; group 2: (LHB + intraorally harvested peripheral AB [IHPB] from retromolar/chin region + BBM, ratio: 1:4), 22 patients, 29 SFEs; and group 3 (LHB + extraorally harvested peripheral AB [EHPB] from iliac crest/tibia + BBM, ratio 1:1), 28 patients, 53 SFEs. After graft healing (5 to 7 months), 284 dental implants (group 1: 76, group 2: 61, group 3: 147 [overall: 2.3 implants/sinus]) were placed. After an additional healing period (5 to 7 months), all implants placed were functionally loaded and prospectively followed by clinical and radiographic evaluations assessing implant survival/success rate as well as peri-implant marginal bone level (MBL) alteration at 1, 3, and 5 years postloading.
Results: A total of 76/81 patients with 267/284 implants were followed for up to 5 years (dropouts: 5 patients/ 15 implants; implant loss = 2). The 5-year implant survival and implant success rate (group 1: 100%/98.6%; group 2: 98.3%/96.6%; group 3: 99.3%/95.7%) did not differ between the three graft mixture groups. The peri-implant marginal bone alteration (reduction) averaged over all 5 years was 1.40 ± 0.29 mm for group 1, 1.41 ± 0.22 mm for group 2, and 1.46 ± 0.46 mm for group 3 (P = .187). However, over time, a continual and significant MBL reduction (P = .045) was noted for all groups presenting peri-implant MBL changes between 1 year and 5 years of -0.17 mm (group 1), -0.12 mm (group 2), and -0.24 mm (group 3), respectively.
Conclusion: According to the clinical results obtained, dental implants inserted in grafted (staged) SFE using a mixture of BBM with a minimal amount of AB harvested from local sites provide for similarly high 5-year implant/augmentation success rates as graft mixtures with AB harvested from peripheral intraoral or extraoral donor sites, confirming no need for additional bone harvesting.
Schlagwörter: 3 different bone ratios, implant survival/success, staged maxillary sinus augmentation
International Journal of Oral Implantology, 2/2014
PubMed-ID: 24977253Seiten: 173-184, Sprache: EnglischKrennmair, Stefan / Seemann, Rudolf / Weinländer, Michael / Krennmair, Gerald / Piehslinger, Eva
Objectives: To evaluate the outcome of immediately loaded distally cantilevered mandibular full-arch prostheses according to the 'all-on-four' concept supported by implants placed in both fresh extraction and healed sites.
Material and methods: A prospective study was conducted in 24 patients with extraction of all remaining mandibular teeth and placement of 4 implants per patient (2 mesial axial and 2 distal tilted) for full-arch mandibular restorations. Implants were inserted in fresh extraction sockets 2.3 ± 1.0 per patient and 1.7 ± 1.0 implants in healed sites. Implants placed in fresh extraction sites (n = 55) were significantly (P
Schlagwörter: edentulous mandible, extraction sites, fixed full arch prostheses, immediate implant placement, immediate loading
Conflict of interest statement: Prof Gerald Krennmair was supported by a grant from Camlog Foundation to conduct this research.
The International Journal of Oral & Maxillofacial Implants, 3/2013
DOI: 10.11607/jomi.3024, PubMed-ID: 23748316Seiten: 831-840, Sprache: EnglischKrennmair, Gerald / Seemann, Rudolf / Weinländer, Michael / Krennmair, Stefan / Piehslinger, Eva
Purpose: This retrospective study evaluated implant and prosthodontic survival/success rates of four-implant- supported distal cantilevered mandibular fixed prostheses over more than 5 years of clinical use.
Materials and Methods: Patients with mandibular edentulism treated with four-implant mandibular prostheses with distal extensions were evaluated. Cumulative implant survival/success rates, peri-implant conditions, and prosthodontic maintenance efforts were assessed. Relationships between the degree of distal implant tilting, length of cantilevers, and implant-generated supporting zone were evaluated.
Results: Thirty-eight patients with 152 implants (90.5% of the original sample) were available for follow-up after 5 to 7 years (mean follow-up, 66.5 ± 3.1 months). The cumulative survival and success rates for included implants were 100% and 98.6%, respectively. Denture cantilever length (mean, 14.7 ± 2.3 mm; range, 9 to 20 mm) and implant-generated supporting zone (mean, 318.9 ± 48.1 mm2; range, 225 to 410 mm2) showed significant positive and negative correlations, respectively, with the inclination of tilted distal implants toward the occlusal plane (76 ± 7.2 degrees; range, 65 to 90 degrees). Peri-implant marginal bone resorption (1.5 ± 0.4 mm) and pocket depths (1.8 ± 0.8 mm) were similar for anterior and posterior implants and were not influenced by degree of tilting or cantilever length. Plaque and calculus conditions were poorer for anterior implants than for posterior implants. No dentures fractured; however, fractures of resin tooth veneer material, denture rebasing, and a strong need for cleaning as a result of resin discoloration were seen.
Conclusion: Fixed four-implant rehabilitations with distal cantilevers of a defined length with or without distally tilted implants showed high success rates. Inferior hygiene in the anterior mandible regions may be a result of reduced cleansability and variations in anatomical landmarks. Resin veneering proved advantageous for repair or modification but disadvantageous for discoloration.
The International Journal of Oral & Maxillofacial Implants, 5/2011
PubMed-ID: 22010088Seiten: 1043-1050, Sprache: EnglischKrennmair, Gerald / Seemann, Rudolf / Weinländer, Michael / Wegscheider, Walther / Piehslinger, Eva
Purpose: The aim of this retrospective study was to evaluate implant survival/success rates and peri-implant parameters as well as patient satisfaction for uniformly designed implant-supported anterior maxillary or mandibular fixed partial dentures (FPDs).
Materials and Methods: A retrospective study was conducted on patients with maxillary or mandibular anterior partial edentulism (all incisors missing) treated between 2002 and 2006 with a two-implant-supported four-unit FPD. All FPDs were of the same design: two implant abutments in the lateral incisor positions and two ovate pontics in the central incisor positions. Cumulative implant survival rates and peri-implant conditions (marginal bone loss, pocket depth, Plaque Index, Gingival Index, Bleeding Index, Periotest values) as well as the incidence and type of prosthodontic maintenance were evaluated. The patients' subjective satisfaction rate was surveyed using multiple questionnaires with a 10-point scoring system (0 = not satisfied to 10 = highly satisfied).
Results: Thirty-six of 38 patients (dropout: 5%) with 72 implants (50 maxillary and 22 mandibular implants, 25 maxillary and 11 mandibular FPDs) were available for follow-up after a mean observation period of 56.2 ± 10.3 months. High cumulative implant survival and success rates (100%) and healthy peri-implant parameters (mean marginal bone resorption: 1.8 ± 0.3 mm; mean pocket depth: 2.5 ± 1.0 mm; Periotest value: -4.5 ± 1.1; and Plaque/Bleeding/Gingival indices of 0 in 70% of sites [with significantly better results in the maxilla than in the mandible]) were achieved. The most frequent required prosthodontic maintenance efforts were maxillary recementation (3/25; 12%) and mandibular rebasing (2/11; 18.2%). A high score for satisfaction was obtained, although slightly better overall results were seen for maxillary than for mandibular FPDs.
Conclusion: For all parameters evaluated, these FPDs proved to be a viable treatment procedure for anterior partial edentulism with good clinical and esthetic outcomes.
Schlagwörter: anterior region, clinical outcome, dental implants, fixed partial dentures, patient satisfaction
The International Journal of Oral & Maxillofacial Implants, 3/2011
PubMed-ID: 21691608Seiten: 598-606, Sprache: EnglischKrennmair, Gerald / Seemann, Rudolf / Weinländer, Michael / Piehslinger, Eva
Purpose: Implant success, peri-implant conditions, and prosthodontic maintenance requirements were evaluated and compared for mandibular overdentures supported by two implants and retained with ball or resilient telescopic crown attachments during a 5-year period.
Materials and Methods: Twenty-five patients with an edentulous mandible each received two root-form dental implants in the mandibular interforaminal (canine) region. The type of denture attachment was chosen randomly; 13 patients received ball attachments and 12 patients received resilient telescopic crowns. Implant success and peri-implant conditions (bone resorption, pocket depth, Plaque Index, Gingival Index, Bleeding Index) as well as prosthodontic maintenance and patient satisfaction were evaluated annually during a 5-year follow-up period and compared with respect to the two retention modalities used.
Results: Implant success, peri-implant conditions, and subjective patient satisfaction scores did not differ between the two retention modalities used. However, during the 5-year observation period, significantly more postinsertion complications/interventions for maintenance purposes were registered in the ball group (87 interventions, 61.1%) than in the telescopic crown group (53 interventions, 37.9%; P < .01). Differences in prosthodontic maintenance efforts were most significant in the second and third years (P < .05) of the follow-up period but were similar at the end of the study for both anchorage systems.
Conclusion: Both ball attachments and resilient telescopic crowns on isolated implants in the atrophic mandible are viable treatment options for implant-supported overdentures. No implant losses, good peri-implant conditions, and general patient satisfaction were noted. Although the frequency of technical complications was initially higher with ball attachments than with resilient telescopic crowns over a 5-year period, similar frequencies of maintenance efforts may be anticipated for both retention modalities.
Schlagwörter: ball anchors, implant-retained prostheses, mandibular overdentures, prosthodontic maintenance, telescopic crowns
The International Journal of Oral & Maxillofacial Implants, 3/2010
PubMed-ID: 20556260Seiten: 589-597, Sprache: EnglischWeinländer, Michael / Piehslinger, Eva / Krennmair, Gerald
Purpose: The present study evaluated implant and peri-implant outcomes as well as prosthodontic maintenance efforts for implant/bar-supported mandibular prostheses with different prosthesis anchorage systems.
Materials and Methods: Seventy-six patients who received two or four interforaminal implants were assigned to one of three different bar designs and subsequently to different prosthesis supporting systems. Forty-nine patients received implants and a mucosa-supported implant-retained overdenture (OD) with an ovoid bar (two implants; design 1) or multiple ovoid bars (four implants; design 2). Twenty-seven patients received four implants and a rigid implant-supported prosthesis (ISP) with a milled bar (design 3). Implant survival, peri-implant parameters (marginal bone resorption, pocket depth, and plaque, bleeding, gingival, and calculus indices), and postinsertion prosthodontic maintenance were followed over a 5-year period and compared among the different retention modalities. At the most recent follow-up examination, subjective patient satisfaction was additionally evaluated using a simplified scoring system (ranging from 1 = not satisfactory to 5 = excellent).
Results: Implant survival rates (100%) and all peri-implant parameters evaluated showed no differences among the three designs used for implant prosthesis anchorage. Prosthodontic maintenance did not differ between the different ODs (OD design 1: average of 1.04 maintenance visits/year/patient; OD design 2: 1.2 maintenance visits/year/patient), but it was significantly lower for the dentures that were rigidly stabilized with milled bars (ISP: 0.37 maintenance visits/year/patient). A high subjective satisfaction rate (range: 4.5 to 5.0) was registered at the final examination, without any differences among the designs used.
Conclusions: Rigid anchorage with milled bars on four-implant prostheses combined with a metal-reinforced framework showed a lower extent of prosthodontic maintenance issues than round bars on two- or four-implant overdentures with resilient denture stabilization. Nevertheless, implants and peri-implant structures were not negatively affected by either resilient or rigid anchorage mechanisms.
Schlagwörter: edentulous mandible, implant-supported overdentures, milled bar, prosthodontic maintenance, round bar