The International Journal of Oral & Maxillofacial Implants, Pre-Print
DOI: 10.11607/jomi.10780, PubMed ID (PMID): 3839444123. Feb 2024,Language: EnglishReinedahl, David / Galli, Silvia / Albrektsson, Tomas / Tengvall, Penni / Wennerberg, Ann
Purpose: Marginal bone resorption (MBR) around oral implants may sometimes be a selflimiting
condition due to balancing immunological reactions against the utilized materials,
rather than a progressive bacterial infection. Contrary to previous assumptions from ligature
induced experimental peri-implantitis studies, our recent 8-week experiment showed that
marginal ligatures per se trigger an inflammatory immune response, resulting in bone
resorption around implants in absence of a plaque. The present study aims to investigate
whether this inflammatory/immunological reaction attenuates or progresses toward implant
failure after a longer healing time, 12 weeks. Materials and Methods: Sterile silk ligatures
were placed around the top of titanium (Ti) implants and compressed against the femoral
cortical bone plate of 6 rabbits. A non-ligated implant was used as control. After 12 weeks of
submerged healing, ground sections of implants and surrounding tissues were investigated
with light microscopy. The marginal soft tissues were also analyzed using selected qPCR
markers. Results: Histologically, the ligatures were outlined by immune cells, including
multinucleated giant cells (MNGC), with adjacent fibrous encapsulation and resorbed
peripheral bone that contrasted from the osseointegrated non-ligated control implants. The
difference in expression of qPCR markers was not significant, but >2-fold upregulation of
markers CD11b, IL1b, ARG1, NCF1, CD4 and >2-fold downregulation of CD8 indicated a
mild, focal inflammatory/immune response against the ligatures compared to controls, with
upregulation of M1 and M2 macrophages, neutrophils and helper T-cells and downregulation
of killer T cells. Further, the bone formation markers OC and ALPL were >2 fold down
regulated, consistent with the lack of osseointegration of the ligatures, compared to control
implants. Conclusions: Marginal silk ligatures per se trigger an inflammatory/immune
response and aseptic bone resorption around oral implants. Compared to our previous 8-week
study, the inflammatory reaction against the silk appears to attenuate with time, with only a
mild persisting inflammation that may block osseointegration and instead maintains a fibrous
tissue encapsulation type reaction. This may explain why traditional ligature experiments
have required regular exchange of ligatures in order for the bone resorption to progress.
The International Journal of Oral & Maxillofacial Implants, Pre-Print
DOI: 10.11607/jomi.10820, PubMed ID (PMID): 3849879018. Mar 2024,Pages 1-27, Language: EnglishAmengual, Luis / Brañes, Manuel / Marchesani, Francisco / Parada, Leopold / Jara, Maria Constanza / Albrektsson, Tomas
Purpose: To evaluate the feasibility of reversing a primary failure through therapeutic mechanical stimulation induced by transcutaneous application of acoustic waves (ESWT) in the peri-implant tissues. Materials and Μethods: This clinical report evaluates the outcome of a new protocol proposed to treat a primary failure (loosened oral implant); application of three cycles of ESWT, once session per week for 3 consecutive weeks, with an equivalent positive energy of 0,18 mJ/mm² (therapeutic dose: 2000 impulses/ 8Hz/ 4.0 bar). Standardized intraoral radiographs, Cone Beam Computed Tomography (CBCT), Implant Stability Quotient (ISQ) and clinical evaluations were performed. Results: It was possible to verify a progressive increase in the ISQ value after the ESWT protocol; 17 (initial), 46 (after two months) and 68 (after four months), which led to successful implant prosthetic rehabilitation (35 N/cm measured). Our evaluation at 6 years of follow-up confirms that the new bone-implant interface is preserved and ESWT as a safe non-invasive treatment. Conclusion: In the context of the new dynamic model of osseointegration, the Foreign Body Equilibrium (FBE), this represents the first report of a host-Implant equilibrium re-established after an early failure process. However, it is necessary to perform studies to determine both the medical device and the most effective therapeutic range for clinical applications of this technology in oral implantology.
Keywords: ESWT, primary failure, case report, osseointegration, oral implant, osteoimmunology
The International Journal of Oral & Maxillofacial Implants, 5/2023
DOI: 10.11607/jomi.10694, PubMed ID (PMID): 37847825Pages 838-840, Language: EnglishJensen, Ole T. / Albrektsson, Tomas / Jemt, Torsten
The International Journal of Oral & Maxillofacial Implants, 5/2021
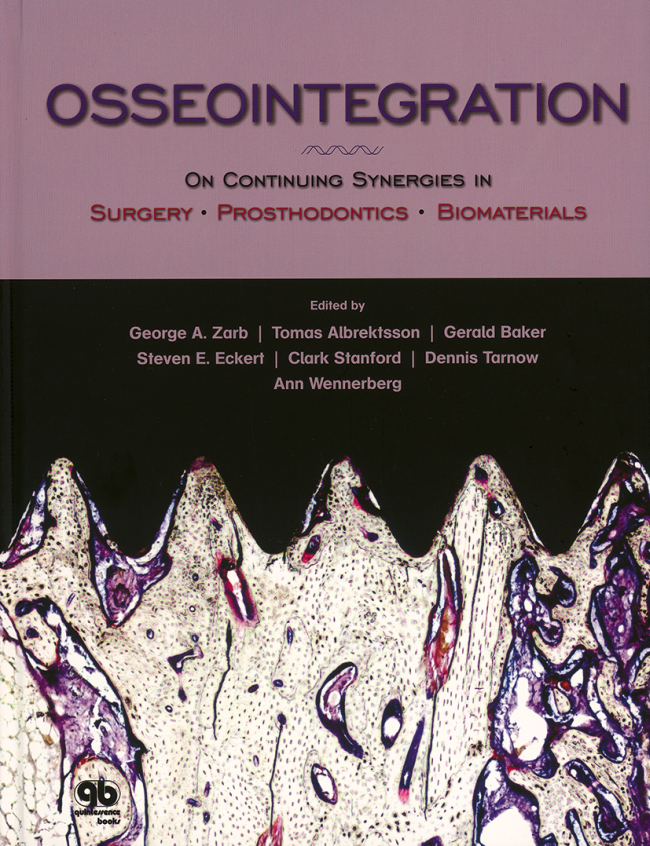
DOI: 10.11607/jomi.8837Pages 863-874, Language: EnglishDuddeck, Dirk U / Albrektsson, Tomas / Wennerberg, Ann / Larsson, Christel / Mouhyi, Jaafar / Beuer, Florian
Purpose: After some initial setbacks in the 1970s, ceramic implants seem to be a promising alternative to titanium implants. Since the surface of an implant system represents the interface to surrounding biologic structures, the study focuses on cleanliness and surface topography. Clinical documentation of the corresponding systems completes the picture and allows a better evaluation of zirconia implant systems.
Materials and methods: Five different ceramic implant systems were selected randomly and purchased via blind-shopping: Z5s (Z-Systems), ZiBone (COHO), W implant (TAVDental), ceramic. implant (vitaclinical), and BioWin!/Standard Zirkon Implantat (Champions-Implants/ZV3 system). Three samples of each implant system underwent scanning electron microscopy (SEM) imaging and elemental analysis (EDS). Where appropriate, subsequent Time-of-Flight Secondary Ion Mass Spectrometry (ToF-SIMS) was performed to identify the chemical nature of impurities. Surface topography was evaluated, and a search for clinical trials in the PubMed database, on the websites and by written request to each dental implant manufacturer, was performed.
Results: Surfaces of Champions implants (ZV3) and Z-Systems implants were relatively clean, whereas the other investigated surfaces of vitaclinical, TAV Dental, and ZiBone implants all displayed organic contaminations on their surfaces. Four of the investigated ceramic implants showed a moderately rough implant surface. Only the vitaclinical ceramic.implant had minimal surface roughness. Three ceramic designs-vitaclinical, ZV3, and Z-Systems-had clinical trials documented with up to 3 years of follow-up and results varying between 82.5% and 100% survival. TAV Dental W and ZiBone implant systems lacked properly conducted clinical recording of results.
Conclusion: The results of this study showed that it is technically possible to produce zirconia implants that are largely residue-free. On the other hand, the variety of significant residues found in this analysis raises concerns, as contamination may lead to undesirable biologic effects. The lack of clinical studies in peer-reviewed journals does not seem to be relevant for the approval of marketing, nor does the lack of surface cleanliness. In the authors' opinion, a critical analysis of these aspects should be included in a more stringent future analysis prior to the marketing of oral implant systems.
Keywords: ceramic implants, dental implants, implant contamination, implant surface, scanning electron microscopy, surface, surface properties, zirconia
The International Journal of Prosthodontics, 5/2020
DOI: 10.11607/ijp.6701, PubMed ID (PMID): 32956432Pages 513-522, Language: EnglishGjelvold, Björn / Kisch, Jenö / Mohammed, Deyar Jallal Hadi / Chrcanovic, Bruno Ramos / Albrektsson, Tomas / Wennerberg, Ann
Purpose: To compare clinical and esthetic outcomes between immediately loaded single implants placed with and without a fully guided surgical procedure.
Materials and Methods: Patients with a missing maxillary tooth (second premolar to second premolar) were considered for inclusion in this 1-year prospective nonrandomized study. Exclusion criteria were general health contraindications for oral surgery besides the need for bone grafting or ridge augmentation. One group received digital implant planning, fully guided surgery, and immediate loading (DIL). The other group received freehand surgery and immediate loading (IL). Outcome measures were implant survival, marginal bone loss, soft tissue changes, papilla index, pink and white esthetic scores (PES and WES, respectively), and patient-reported outcome measures (PROMs).
Results: Two of 21 implants failed in the DIL group soon after placement, resulting in a 1-year implant survival rate of 90.5%, while no implants failed in the IL group. Significantly higher papilla index scores and lower soft tissue changes were found for the DIL group compared to the IL group. No differences were found after 1 year regarding marginal bone loss, PES, WES, or PROMs.
Conclusion: Within the limitations of this study, immediate loading in combination with fully guided surgery might negatively affect implant survival. Immediate loading, fully guided surgery, and a digital workflow appear to have a positive effect on early soft tissue adaptation.
The International Journal of Oral & Maxillofacial Implants, 3/2020
DOI: 10.11607/jomi.8218, PubMed ID (PMID): 32406645Pages 495-502, Language: EnglishAlbrektsson, Tomas / Dahlin, Christer / Reinedahl, David / Tengvall, Pentti / Trindade, Ricardo / Wennerberg, Ann
Purpose: The purpose of this paper is to present evidence that supports the notion that the primary reason behind marginal bone loss and implant failure is immune-based and that bacterial actions in the great majority of problematic cases are of a secondary nature.
Materials and Methods: The paper is written as a narrative review.
Results: Evidence is presented that commercially pure titanium is not biologically inert, but instead activates the innate immune system of the body. For its function, the clinical implant is dependent on an immune/inflammatory defense against bacteria. Biologic models such as ligature studies have incorrectly assumed that the primary response causing marginal bone loss is due to bacterial action. In reality, bacterial actions are secondary to an imbalance of the innate immune system caused by the combination of titanium implants and ligatures, ie, nonself. This immunologic imbalance may lead to marginal bone resorption even in the absence of bacteria.
Conclusion: Marginal bone loss and imminent oral implant failure cannot be properly analyzed without a clear understanding of immunologically caused tissue responses.
Keywords: biomaterials, failure analysis, immunologic reactions, peri-implantitis, review (narrative)
The International Journal of Oral & Maxillofacial Implants, 2/2020
DOI: 10.11607/jomi.7488, PubMed ID (PMID): 32142574Pages 366-378, Language: EnglishAparicio, Carlos / López-Piriz, Roberto / Albrektsson, Tomas
Zygomatic-related implant rehabilitation differs from traditional implant treatment in biomechanics, clinical procedures, outcomes, and eventual complications such as soft tissue incompetence or recession that may lead to recurrent sinus/soft tissue complications. The extreme maxillary atrophy that indicates the use of zygomatic implants prevents use of conventional criteria to describe implant success/failure. Currently, results and complications of zygomatic implants reported in the literature are inconsistent and lack a standardized systematic review. Moreover, protocols for the rehabilitation of the atrophic maxilla using zygomatic implants have been in continuous evolution. The current zygomatic approach is relatively new, especially if the head of the zygomatic implant is located in an extramaxillary area with interrupted alveolar bone around its perimeter. Specific criteria to describe success/survival of zygomatic implants are necessary, both to write and to read scientific literature related to zygomatic implant–based oral rehabilitations. The aim of this article was to review the criteria of success used for traditional and zygomatic implants and to propose a revisited Zygomatic Success Code describing specific criteria to score the outcome of a rehabilitation anchored on zygomatic implants. The ORIS acronym is used to name four specific criteria to systematically describe the outcome of zygomatic implant rehabilitation: offset measurement as evaluation of prosthetic positioning; rhino-sinus status report based on a comparison of presurgical and postsurgical cone beam computed tomography in addition to a clinical questionnaire; infection permanence as evaluation of soft tissue status; and stability report, accepting as success some mobility until dis-osseointegration signs appear. Based on these criteria, the assessment of five possible conditions when evaluating zygomatic implants is possible.
Keywords: criteria of success, ORIS, review (narrative), ZAGA, zygomatic implants, zygomatic success code
The International Journal of Prosthodontics, 7/2018
SupplementPages 11-14, Language: EnglishAlbrektsson, Tomas
The International Journal of Prosthodontics, 5/2018
Pages 420-422, Language: EnglishAlbrektsson, Tomas / Zarb, George
International Journal of Oral Implantology, 5/2018
SupplementPubMed ID (PMID): 30109294Pages S9-S13, Language: EnglishAlbrektsson, Tomas / Goodacre, Charles / Jacobs, Reinhilde / Jerjes, Waseem / Korfage, Anke / Larsson, Christel / Neukam, Friedrich / Packer, Mark / Pommer, Bernhard / van Steenberghe, Daniel / Veitz-Keenan, Analia / Wennerberg, Ann
Diagnosis, avoidance and management of complications of implant-based treatments